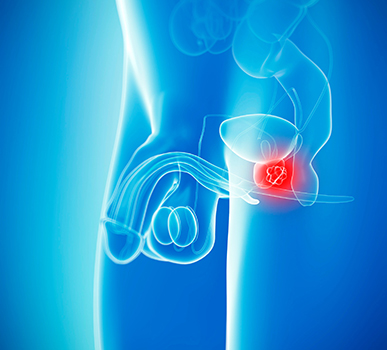
What is Prostate Cancer?
Cancer starts when cells in the body begin to grow out of control. Cells in nearly any part of the body can become cancer cells, and can then spread to other areas of the body. Prostate cancer is cancer that occurs in the prostate - a small walnut-shaped gland in men that produces the seminal fluid that nourishes and transports sperm. Prostate cancer is one of the most common types of cancer in men. Usually prostate cancer grows slowly and is initially confined to the prostate gland, where it may not cause serious harm. Prostate cancer begins when cells in the prostate gland start to grow out of control.
What causes prostate cancer?
On a basic level, prostate cancer is caused by changes in the DNA of a normal prostate cell. DNA is the chemical in our cells that makes up our genes, which control how our cells function. Cancer can be caused by DNA mutations (or other types of changes) that keep oncogenes turned on, or that turn off tumor suppressor genes. These types of gene changes can lead to cells growing out of control. DNA changes can either be inherited from a parent or can be acquired during a person's lifetime.
We at CAN-C provide prostate cancer treatment in Bangalore.
Here, you will find information about signs and symptoms, causes and risk factors, types, diagnosis, staging and prevention about prostate cancer.
Most prostate cancers are found early, through screening. Early prostate cancer usually causes no symptoms. More advanced prostate cancers can sometimes cause symptoms, such as:
Problems urinating, including a slow or weak urinary stream or the need to urinate more often, especially at night
Blood in the urine or semen
Trouble getting an erection (erectile dysfunction or ED)
Pain in the hips, back (spine), chest (ribs), or other areas from cancer that has spread to bones
Weakness or numbness in the legs or feet, or even loss of bladder or bowel control from cancer pressing on the spinal cord
Pain or burning when you pee
Pressure or pain in your rectum
CAN-C: One-stop centre for prostate cancer treatment in Bangalore.
A risk factor is anything that raises your risk of getting a disease such as cancer. Different cancers have different risk factors. Several factors that might affect a man's risk of getting prostate cancer are listed below:
Age: The chance of having prostate cancer rises rapidly after age 50.
Family history: Prostate cancer seems to run in some families, which suggests that in some cases there may be an inherited or genetic factor. Still, most prostate cancers occur in men without a family history of it.
Gene changes: Several inherited gene changes (mutations) seem to raise prostate cancer risk, but they probably account for only a small percentage of cases overall.
Men with Lynch syndrome (also known as hereditary non-polyposis colorectal cancer, or HNPCC): a condition caused by inherited gene changes, have an increased risk for a number of cancers, including prostate cancer.
Obesity: Being obese (very overweight) does not seem to increase the overall risk of getting prostate cancer.
Smoking: Smoking increases the risk of getting prostate cancer.
Chemical exposures: Exposing to chemicals that may increase their risk of prostate cancer.
Inflammation of the prostate: Prostatitis (inflammation of the prostate gland) may be linked to an increased risk of prostate cancer.
Types of prostate cancer are:
Almost all prostate cancers are adenocarcinomas. Adenocarcinomas are cancers that develop in the gland cells that line the prostate gland. They are the most common type of prostate cancer. Nearly everyone with prostate cancer has this type. As mentioned, adenocarcinomas make up the vast majority of prostate cancer cases.
Acinar adenocarcinomas: It develops in acini cells and increase PSA (prostate-specific antigen) levels. These cells form clusters and line fluid secreting glands. In the prostate, acini line the gland and produce the fluid that will eventually become semen.
Ductal adenocarcinoma: It starts in the cells that line the tubes and ducts of the prostate gland, and doesn't always impact PSA levels, making it potentially harder to detect. In addition, ductal adenocarcinomas often spread faster than acinar adenocarcinomas.
Other types of cancer that can start in the prostate include:
1. Small cell carcinomas
2. Neuroendocrine tumors (other than small cell carcinomas)
3. Transitional cell carcinomas
4. Sarcomas
These other types of prostate cancer are rare. If you are told you have prostate cancer, it is almost certain to be an adenocarcinoma.
We at CAN-C are here to provide the latest prostate cancer treatments (in Bangalore) alongside the best possible care.
The diagnosis of prostate cancer include.
Medical history and physical exam: If your doctor suspects you might have prostate cancer, he or she will ask you about any symptoms you are having, such as any urinary or sexual problems, and how long you have had them.
PSA blood test: Prostate-specific antigen (PSA) is a protein made by cells in the prostate gland (both normal cells and cancer cells). PSA is mostly in semen, but a small amount is also in the blood.
Prostate biopsy: If the results of a PSA blood test, DRE, or other tests suggest that you might have prostate cancer, your will most likely need a prostate biopsy.
Genetic testing for some men with prostate cancer: Some men with prostate cancer be tested to look for certain inherited gene changes. This includes men in whom a family cancer syndrome (such as a BRCA gene mutation or Lynch syndrome) is suspected, as well as men with prostate cancer that has certain high-risk features or that has spread to other parts of the body.
Imaging tests for prostate cancer: Imaging tests use x-rays, magnetic fields, sound waves, or radioactive substances to create pictures of the inside of your body. One or more imaging tests might be used: To look for cancer in the prostate, to help the doctor see the prostate during certain procedures, to look for spread of prostate cancer to other parts of the body. The imaging tests used most often to look for prostate cancer spread include: Transrectal ultrasound (TRUS), Magnetic resonance imaging (MRI), Bone scan, Computed tomography (CT) scan.
Lymph node biopsy: In a lymph node biopsy, also known as lymph node dissection or lymphadenectomy, one or more lymph nodes are removed to see if they have cancer cells. This isn't done very often for prostate cancer, but it might be used to find out if the cancer has spread from the prostate to nearby lymph nodes.
The stage of a prostate cancer describes how much cancer is in the body. It helps determine how serious the cancer is and how best to treat it. The stage is based on tests described in Tests to Diagnose and Stage Prostate Cancer, including the blood PSA level and prostate biopsy results.
A staging system is a standard way to describe how far a cancer has spread. The most widely used staging system for prostate cancer is the TNM system.
The TNM system for prostate cancer is based on 3 key pieces of information:
The extent of the main (primary) tumor (T category)
Whether the cancer has spread to nearby lymph nodes (N category)
Whether the cancer has spread (metastasized) to other parts of the body (M category)
In Bangalore, we at CAN-C are passionate about delivering exceptional treatment to all people living with prostate cancer.
There is no sure way to prevent prostate cancer. But, there are some things you can do that might lower your risk of prostate cancer and are listed below:
Body weight, physical activity, and diet: The effects of body weight, physical activity, and diet on prostate cancer risk are not clear, but there are things you can do that might lower your risk.
Vitamin, mineral, and other supplements: Vitamin E and selenium: Taking vitamin E or selenium supplements might lower prostate cancer risk.
Stop smoking and drink less: Quitting smoking can improve your health in many ways, including lowering your cancer risk. And if you drink, do so in moderation.
"CAN-C: Expert in providing top-quality treatment (in Bangalore) for prostate cancer."
Make An Appointment Today
How Prostate Cancer is treated?
The treatment for prostate cancer depends on: where your cancer is, how far it has grown or spread (the stage), the type of cancer, how abnormal the cells look under a microscope (the grade), your general health and level of fitness. Depending on each case, treatment options for men with prostate cancer might include:
Surgery is a common choice to try to cure prostate cancer if it is not thought to have spread outside the prostate gland. The main type of surgery for prostate cancer is a radical prostatectomy. In this operation, the surgeon removes the entire prostate gland plus some of the tissue around it, including the seminal vesicles.
Open or laparoscopic radical prostatectomy:
In the more traditional approach to prostatectomy, called an open prostatectomy, the surgeon operates through a single long skin incision (cut) to remove the prostate and nearby tissues.
In a laparoscopic prostatectomy, the surgeon makes several smaller incisions and uses special long surgical tools to remove the prostate. The surgeon either holds the tools directly, or uses a control panel to precisely move robotic arms that hold the tools. This approach to prostatectomy has become more common in recent years. If done by experienced surgeons, the laparoscopic radical prostatectomy can give results similar to the open approach.
1. Open prostatectomy:
Radical retropubic prostatectomy: For this open operation, the surgeon makes an incision (cut) in your lower abdomen, from the belly button down to the pubic bone.
Radical perineal prostatectomy: In this open operation, the surgeon makes the cut (incision) in the skin between the anus and scrotum (the perineum). This approach is used less often because it's more likely to lead to erection problems and because the nearby lymph nodes can't be removed.
2. Laparoscopic prostatectomy:
Laparoscopic radical prostatectomy: For a laparoscopic radical prostatectomy (LRP), the surgeon inserts special long instruments through several small incisions in the abdominal wall to remove the prostate. One of the instruments has a small video camera on the end, which lets the surgeon see inside the body.
Robotic-assisted laparoscopic radical prostatectomy: In this approach, also known as robotic prostatectomy, the laparoscopic surgery is done using a robotic system. The surgeon sits at a control panel in the operating room and moves robotic arms to operate through several small incisions in the patient's abdomen.
3. Transurethral resection of the prostate (TURP): This operation is more often used to treat men with non-cancerous enlargement of the prostate called benign prostatic hyperplasia (BPH). But it is also sometimes used in men with advanced prostate cancer to help relieve symptoms, such as trouble urinating. (It is not used to try to cure the cancer.)
We provide specialized prostate cancer treatment (in Bangalore) that has been targeted to individual patient characteristics.
Radiation therapy uses high-energy rays or particles to kill cancer cells. Depending on the stage of the prostate cancer and other factors, radiation therapy might be used:
1. As the first treatment for cancer that is still just in the prostate gland and is low grade. Cure rates for men with these types of cancers are about the same as those for men treated with radical prostatectomy.
2. As part of the first treatment (along with hormone therapy) for cancers that have grown outside the prostate gland and into nearby tissues.
3. If the cancer is not removed completely or comes back (recurs) in the area of the prostate after surgery.
4. If the cancer is advanced, to help keep the cancer under control for as long as possible and to help prevent or relieve symptoms.
Types of radiation therapy:
The main types of radiation therapy used for prostate cancer are:
1. External beam radiation: In EBRT, beams of radiation are focused on the prostate gland from a machine outside the body. This type of radiation can be used to try to cure earlier stage cancers, or to help relieve symptoms such as bone pain if the cancer has spread to a specific area of bone.
Three-dimensional conformal radiation therapy (3D-CRT): 3D-CRT uses special computers to precisely map the location of your prostate. Radiation beams are then shaped and aimed at the prostate from several directions, which makes it less likely to damage surrounding normal tissues and organs.
Intensity modulated radiation therapy (IMRT): IMRT, an advanced form of 3D-CRT therapy, is the most common type of external beam radiation therapy for prostate cancer. It uses a computer-driven machine that moves around the patient as it delivers radiation. Along with shaping the beams and aiming them at the prostate from several angles, the intensity (strength) of the beams can be adjusted to limit the doses of radiation reaching nearby normal tissues.
Stereotactic body radiation therapy (SBRT): This technique uses advanced image guided techniques to deliver large doses of radiation to a precise area, such as the prostate.
Proton beam radiation therapy: Proton beam therapy focuses beams of protons instead of x-rays on the cancer. This means that proton beam radiation can, in theory, deliver more radiation to the prostate while doing less damage to nearby normal tissues. Proton beam radiation can be aimed with techniques similar to 3D-CRT and IMRT.
2. Brachytherapy (internal radiation): Brachytherapy (also called seed implantation or interstitial radiation therapy) uses small radioactive pellets, or "seeds," each about the size of a grain of rice. These pellets are placed directly into your prostate.
Brachytherapy alone is generally used only in men with early-stage prostate cancer that is relatively slow growing (low-grade).
Brachytherapy combined with external radiation is sometimes an option for men who have a higher risk of the cancer growing outside the prostate.
There are 2 types of prostate brachytherapy:
Permanent (low dose rate, or LDR) brachytherapy: In this type, pellets (seeds) of radioactive material (such as iodine-125 or palladium-103) are placed inside thin needles, which are inserted through the skin in the area between the scrotum and anus and into the prostate. Radiation from the seeds travels a very short distance, so the seeds can give off a large amount of radiation in a very small area. This limits the amount of damage to nearby healthy tissues.
Temporary (high dose rate, or HDR) brachytherapy: This technique is done less often. It leaves higher doses of radiation in place for a short time. Hollow needles are placed through the skin between the scrotum and anus and into the prostate. Soft nylon tubes (catheters) are placed in these needles. The needles are then removed but the catheters stay in place.
Chemotherapy (chemo) uses anti-cancer drugs injected into a vein or given by mouth. These drugs travel through the bloodstream to reach cancer cells in most parts of the body.
Chemo is sometimes used if prostate cancer has spread outside the prostate gland and hormone therapy isn't working. Chemo might be helpful if given along with hormone therapy.
Chemo drugs used to treat prostate cancer: For prostate cancer, chemo drugs are typically used one at a time. Some of the chemo drugs used to treat prostate cancer include: Docetaxel (Taxotere), Cabazitaxel (Jevtana), Mitoxantrone (Novantrone), Estramustine (Emcyt)
Chemo drugs for prostate cancer are typically given into a vein (IV), either as an infusion over a certain period of time. Some drugs, such as estramustine, are given as a pill.
In Bangalore, our team of experts offer prostate cancer treatment plans suited for patients' needs.
Hormone therapy is also called androgen suppression therapy. The goal is to reduce levels of male hormones, called androgens, in the body, to stop them from fueling prostate cancer cells.
Androgens stimulate prostate cancer cells to grow. The main androgens in the body are testosterone and dihydrotestosterone (DHT). Most androgen is made by the testicles, but the adrenal glands (glands that sit above your kidneys) as well as the prostate cancer itself, can also make a fair amount. Lowering androgen levels or stopping them from getting into prostate cancer cells often makes prostate cancers shrink or grow more slowly for a time.
Hormone therapy may be used:
1. If the cancer has spread too far to be cured by surgery or radiation, or if you can't have these treatments for some other reason
2. If the cancer remains or comes back after treatment with surgery or radiation therapy
3. Along with radiation therapy as the initial treatment, if you are at higher risk of the cancer coming back after treatment
4. Before radiation to try to shrink the cancer to make treatment more effective
Several types of hormone therapy can be used to treat prostate cancer.
1. Treatment to lower testicular androgen levels: Androgen deprivation therapy, also called ADT, uses surgery or medicines to lower the levels of androgens made in the testicles.
2. Treatment to lower androgen levels from the adrenal glands: LHRH agonists and antagonists can stop the testicles from making androgens, but cells in other parts of the body, such as the adrenal glands, and prostate cancer cells themselves, can still make male hormones, which can fuel cancer growth. Drugs are available that block the formation of androgens made by these cells. Abiraterone (Zytiga) blocks an enzyme (protein) called CYP17, which helps stop these cells from making androgens.
3. Drugs that stop androgens from working: For most prostate cancer cells to grow, androgens have to attach to a protein in the prostate cancer cell called an androgen receptor. Anti-androgens are drugs that also connect to these receptors, keeping the androgens from causing tumor growth. Anti-androgens are also sometimes called androgen receptor antagonists.
Immunotherapy is the use of medicines to stimulate a person's own immune system to recognize and destroy cancer cells more effectively. Certain types of immunotherapy can be used to treat prostate cancer.
Cancer vaccine: Sipuleucel-T (Provenge) is a cancer vaccine. Unlike traditional vaccines, which boost the body's immune system to help prevent infections, this vaccine boosts the immune system to help it attack prostate cancer cells.
Immune checkpoint inhibitors: An important part of the immune system is its ability to keep itself from attacking the body's normal cells. To do this, it uses "checkpoint" proteins on immune cells, which act like switches that need to be turned on (or off) to start an immune response. Cancer cells sometimes use these checkpoints to keep the immune system from attacking them. But drugs that target these checkpoints hold a lot of promise as cancer treatments.
PD-1 inhibitor: Pembrolizumab (Keytruda) is a drug that targets PD-1, a checkpoint protein on immune system cells called T cells, that normally helps keep these cells from attacking normal cells in the body. By blocking PD-1, this drug boosts the immune response against prostate cancer cells. This drug is given as an intravenous (IV) infusion.
Get high-quality prostate cancer treatment in Bangalore at CAN-C.
Our Doctors
Dr. Dinesh M G
Specialty: Surgical Oncologist & Laparoscopic Oncosurgeon
Dr. Dinesh M G, is an efficient surgeon specialized in oncology committed to the care and improvement of quality of life of cancer patients. His exceptional surgical skills, teamwork and knowledge are laudable. He is skilled in performing various minimal access oncologic surgeries and has mastered complex open surgeries in the field of oncology.
Completing MBBS from KIMS, Bangalore followed by MS - General Surgery from JJM Medical College, Davangere and M. Ch - Surgical Oncology from Kidwai Memorial Institute of Oncology, he has a Fellowship in Minimal Access Oncology from Basavatarakam Indo American Cancer Institute.

