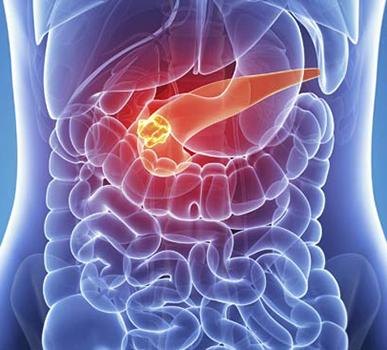
What is Pancreatic Cancer?
Pancreatic cancer is a type of cancer that starts in the pancreas. Pancreatic cancer is a disease in which malignant (cancerous) cells form in the tissues of the pancreas. The pancreas is a gland located behind the stomach and in front of the spine. Pancreatic cancer happens when uncontrolled cell growth begins in a part of the pancreas. Tumors develop, and these interfere with the way the pancreas works.
How pancreatic cancer occurs?
Pancreatic Cancer occurs when damaged cells grow in an uncontrolled way. When the genetic materials that contain instructions for all biochemical processes within the pancreas are damaged or mutated, cancer cells are allowed to replicate. Pancreatic Cancer often starts within the cells of the pancreatic ducts, and these then spread to the rest of the pancreas.
We provide pancreatic cancer treatment in Bangalore.
Here, you will find information about signs and symptoms, causes and risk factors, types, diagnosis, staging and prevention about pancreatic cancer.
Symptoms of pancreatic cancer include:
Jaundice and related symptoms: Jaundice is yellowing of the eyes and skin. Most people with pancreatic cancer (and nearly all people with ampullary cancer) will have jaundice as one of their first symptoms.
Belly or back pain: Pain in the abdomen (belly) or back is common in pancreatic cancer. Cancers that start in the body or tail of the pancreas can grow fairly large and start to press on other nearby organs, causing pain. The cancer may also spread to the nerves surrounding the pancreas, which often causes back pain.
Weight loss and poor appetite: Unintended weight loss is very common in people with pancreatic cancer.
Nausea and vomiting: If the cancer presses on the far end of the stomach it can partly block it, making it hard for food to get through. This can cause nausea, vomiting, and pain that tend to be worse after eating.
Gallbladder or liver enlargement: If the cancer blocks the bile duct, bile can build up in the gallbladder, making it larger.
Blood clots: Sometimes, the first clue that someone has pancreatic cancer is a blood clot in a large vein, often in the leg. This is called a deep vein thrombosis or DVT.
Diabetes: Rarely, pancreatic cancers cause diabetes (high blood sugar) because they destroy the insulin-making cells. Symptoms can include feeling thirsty and hungry, and having to urinate often. More often, cancer can lead to small changes in blood sugar levels that don't cause symptoms of diabetes but can still be detected with blood tests.
CAN-C: Well-known for providing newest and most innovative treatments available for pancreatic cancer in Bangalore.
A risk factor is anything that increases your chance of getting a disease such as cancer. Different cancers have different risk factors. The factors which could put you at risk for developing pancreatic cancer include:
Tobacco use: Smoking is one of the most important risk factors for pancreatic cancer. The risk of getting pancreatic cancer is about twice as high among smokers compared to those who have never smoked. Cigar smoking and the use of smokeless tobacco products also increase the risk.
Being overweight: Being very overweight (obese) is a risk factor for pancreatic cancer. Carrying extra weight around the waistline may be a risk factor even in people who are not very overweight.
Diabetes: Pancreatic cancer is more common in people with diabetes. The reason for this is not known. Most of the risk is found in people with type 2 diabetes.
Chronic pancreatitis: Chronic pancreatitis, a long-term inflammation of the pancreas, is linked with an increased risk of pancreatic cancer. Chronic pancreatitis is often seen with heavy alcohol use and smoking.
Workplace exposure to certain chemicals: Heavy exposure at work to certain chemicals used in some industries may raise a person's risk of pancreatic cancer.
Inherited genetic syndromes: Inherited gene changes (mutations) can be passed from parent to child.
Diet: Some studies have linked pancreatic cancer to diets that are high in red and processed meats and low in fruits and vegetables.
Physical inactivity: Lack of physical activity might increase pancreatic cancer risk.
Types of pancreatic cancer are as follows:
Exocrine cancers are by far the most common type of pancreas cancer.
Pancreatic adenocarcinoma: About 95% of cancers of the exocrine pancreas are adenocarcinomas. These cancers usually start in the ducts of the pancreas. Less often, they develop from the cells that make the pancreatic enzymes, in which case they are called acinar cell carcinomas.
Less common types of exocrine cancer: Other, less common exocrine cancers include adenosquamous carcinomas, squamous cell carcinomas, signet ring cell carcinomas, undifferentiated carcinomas, and undifferentiated carcinomas with giant cells.
Ampullary cancer (carcinoma of the ampulla of Vater): This cancer starts in the ampulla of Vater, which is where the bile duct and pancreatic duct come together and empty into the small intestine. Ampullary cancers often block the bile duct while they're still small and have not spread far. This blockage causes bile to build up in the body, which leads to yellowing of the skin and eyes (jaundice). Because of this, these cancers are usually found earlier than most pancreatic cancers.
We at CAN-C has an excellent track record for pancreatic cancer treatment (in Bangalore) with the use of high technology.
If a person has signs and symptoms that might be caused by pancreatic cancer, certain exams and tests will be done to find the cause. If cancer is found, more tests will be done to help determine the extent (stage) of the cancer, including:
Imaging tests: Imaging tests use x-rays, magnetic fields, sound waves, or radioactive substances to create pictures of the inside of your body.
Computed tomography (CT) scan: The CT scan makes detailed cross-sectional images of your body. CT scans are often used to diagnose pancreatic cancer because they can show the pancreas fairly clearly.
Magnetic resonance imaging (MRI): MRI scans use radio waves and strong magnets instead of x-rays to make detailed images of parts of your body.
Ultrasound: Ultrasound (US) tests use sound waves to create images of organs such as the pancreas.
Cholangiopancreatography: This is an imaging test that looks at the pancreatic ducts and bile ducts to see if they are blocked, narrowed, or dilated. These tests can help show if someone might have a pancreatic tumor that is blocking a duct. They can also be used to help plan surgery.
Positron emission tomography (PET) scan: For a PET scan, you are injected with a slightly radioactive form of sugar, which collects mainly in cancer cells. A special camera is then used to create a picture of areas of radioactivity in the body.
Angiography: This is an x-ray test that looks at blood vessels. A small amount of contrast dye is injected into an artery to outline the blood vessels, and then x-rays are taken.
Blood tests: Several types of blood tests can be used to help diagnose pancreatic cancer or to help determine treatment options if it is found.
Biopsy: Imaging test results may strongly suggest pancreatic cancer, but usually the only way to be sure is to remove a small sample of tumor and look at it under the microscope. This procedure is called a biopsy. Biopsies can be done in different ways.
The stage of a cancer describes how much cancer is in the body. It helps determine how serious the cancer is and how best to treat it.
The staging system used most often for pancreatic cancer is the TNM system which stands for Tumour, Node, Metastasis, and is based on 3 key pieces of information:
The extent of the tumor (T): How large is the tumor and has it grown outside the pancreas into nearby blood vessels?
The spread to nearby lymph nodes (N): Has the cancer spread to nearby lymph nodes? If so, how many of the lymph nodes have cancer?
The spread (metastasized) to distant sites (M): Has the cancer spread to distant lymph nodes or distant organs such as the liver, peritoneum (the lining of the abdominal cavity), lungs or bones?
CAN-C: is one of the top centre for pancreatic cancer treatment in Bangalore.
There is no sure way to prevent pancreatic cancer. But there are things you can do that might lower your risk.
Don't smoke: Smoking is the most important avoidable risk factor for pancreatic cancer. Quitting smoking helps lower risk.
Limit alcohol use: Heavy alcohol use has been tied to pancreatic cancer.
Stay at a healthy weight: Getting to and staying at a healthy weight might also help lower your risk.
Choose a healthy diet: A diet full of colorful fruits and vegetables and whole grains may help reduce your risk of cancer.
Limit exposure to certain chemicals in the workplace: Avoiding workplace exposure to certain chemicals may reduce your risk for pancreatic cancer.
"CAN-C: Expert centre for pancreatic cancer treatment in Bangalore."
Make An Appointment Today
How Pancreatic Cancer is treated?
Once diagnosis is confirmed, treatment plans are based on several factors, such as the stage and location of the cancer, the patient's age and general health state. Treatment options may differ from patient to patient. There are different treatment options for people with pancreatic cancer including surgery, chemotherapy and radiotherapy. If the tumour is advanced and has spread throughout the body, combinations of treatments are used to help relieve symptoms and improve, or help to maintain, quality of life.
Two general types of surgery can be used for pancreatic cancer:
1. Potentially curative surgery:
It is used when the results of exams and tests suggest that it's possible to remove (resect) all the cancer. Studies have shown that removing only part of a pancreatic cancer doesn't help patients live longer, so potentially curative surgery is only done if the surgeon thinks all of the cancer can be removed. This is a very complex surgery and it can be very hard for patients.
Curative surgery is done mainly to treat cancers in the head of the pancreas. Because these cancers are near the bile duct, they often cause jaundice, which sometimes allows them to be found early enough to be removed completely.
Whipple procedure (pancreaticoduodenectomy): This is the most common operation to remove a cancer in the head of the pancreas.
Distal pancreatectomy: In this operation, the surgeon removes only the tail of the pancreas or the tail and a portion of the body of the pancreas. The spleen is usually removed as well.
Total pancreatectomy: This operation removes the entire pancreas, as well as the gallbladder, part of the stomach and small intestine, and the spleen. This surgery might be an option if the cancer has spread throughout the pancreas but can still be removed.
2. Palliative surgery:
It may be done if tests show that the cancer is too widespread to be removed completely. This surgery is done to relieve symptoms or to prevent certain complications like a blocked bile duct or intestine.
Cancers growing in the head of the pancreas can block the common bile duct as it passes through this part of the pancreas. This can cause pain and digestive problems because bile can't get into the intestine. The bile chemicals will also build up in the body, which can cause jaundice, nausea, vomiting, and other problems. There are two main options to relieve bile duct blockage in this situation:
Stent placement: The most common approach to relieving a blocked bile duct does not involve actual surgery. Instead, a stent (small tube, usually made of metal) is put inside the duct to keep it open. This is usually done through an endoscope (a long, flexible tube) while you are sedated.
Bypass surgery: In people who are healthy enough, another option for relieving a blocked bile duct is surgery to reroute the flow of bile from the common bile duct directly into the small intestine, bypassing the pancreas. This typically requires a large incision (cut) in the abdomen, and it can take weeks to recover from this. Sometimes surgery can be done through several small cuts in the abdomen using special long surgical tools. (This is known as laparoscopic or keyhole surgery.)
We are one of the leading providers of care and treatment for people with pancreatic cancer in Bangalore.
Radiation therapy uses high-energy x-rays (or particles) to kill cancer cells. It can be helpful in treating some pancreatic cancers.
When might radiation therapy be used?
1. Radiation might be given after surgery (known as adjuvant treatment) to try to lower the chance of the cancer coming back. The radiation is typically given along with chemotherapy, which is together known as chemoradiation or chemoradiotherapy.
2. For borderline resectable tumors, radiation might be given along with chemotherapy before surgery (neoadjuvant treatment) to try to shrink the tumor and make it easier to remove completely.
3. Radiation therapy combined with chemotherapy may be used as part of the main treatment in people whose cancers have grown beyond the pancreas and can't be removed by surgery (locally advanced/unresectable cancers).
4. Radiation is sometimes used to help relieve symptoms (such as pain) in people with advanced cancers or in people who aren't healthy enough for other treatments like surgery.
How is radiation therapy given?
The type of radiation most often used to treat pancreatic cancer (known as external beam radiation therapy) focuses radiation from a source outside of the body on the cancer.
Getting radiation therapy is much like getting an x-ray, but the radiation is stronger. The procedure itself is painless. Each treatment lasts only a few minutes, although the setup time - getting you into place for treatment - usually takes longer.
Chemotherapy (chemo) is an anti-cancer drug injected into a vein or taken by mouth. These drugs enter the bloodstream and reach almost all areas of the body, making this treatment potentially useful for cancers whether or not they have spread.
When might chemotherapy be used?
Chemo is often part of the treatment for pancreatic cancer and may be used at any stage:
1. Before surgery (neoadjuvant chemotherapy): Chemo can be given before surgery (sometimes along with radiation) to try to shrink the tumor so it can be removed with less extensive surgery. Neoadjuvant chemo is often used to treat cancers that are too big to be removed by surgery at the time of diagnosis (called locally advanced cancers).
2. After surgery (adjuvant chemotherapy): Chemo can be used after surgery (sometimes along with radiation) to try to kill any cancer cells that have been left behind or have spread but can't be seen, even on imaging tests. If these cells were allowed to grow, they could form new tumors in other places in the body. This type of treatment might lower the chance that the cancer will come back later.
3. For advanced pancreatic cancer: Chemo can be used when the cancer is advanced and can't be removed completely with surgery, or if surgery isn't an option, or if the cancer has spread to other organs.
4. When chemo is given along with radiation, it is known as chemoradiation. It helps the radiation work better.
Which chemo drugs are used for pancreatic cancer?
In most cases (especially as adjuvant or neoadjuvant treatment), chemo is most effective when combinations of drugs are used. For people who are healthy enough, 2 or more drugs are usually given together. For people who are not healthy enough for combined treatments, a single drug (usually gemcitabine, 5-FU, or capecitabine) can be used.
The most common drugs used for adjuvant and neoadjuvant chemo include:
Gemcitabine (Gemzar), 5-fluorouracil (5-FU), Oxaliplatin (Eloxatin), Albumin-bound paclitaxel (Abraxane), Capecitabine (Xeloda), Cisplatin, Irinotecan (Camptosar)
Chemo drugs for pancreatic cancer can be given into a vein (IV) or by mouth as a pill.
There is a development of newer drugs to specifically target the changes in pancreatic cancer cells that help them grow. These targeted drugs work differently from standard chemo drugs. Sometimes they work when standard chemo drugs don't.
Erlotinib (Tarceva) is a drug that targets a protein on cancer cells called EGFR, which normally helps the cells grow. In people with advanced pancreatic cancer, this drug can be given along with the chemo drug gemcitabine. Some people may benefit more from this combination than others.
In Bangalore, we are dedicated to providing pancreatic cancer treatment with care of the highest standard.
Immunotherapy is the use of medicines to stimulate a person's own immune system to recognize and destroy cancer cells more effectively. Certain types of immunotherapy can be used to treat pancreatic cancer.
Immune checkpoint inhibitors
An important part of the immune system is its ability to keep itself from attacking the body's normal cells. To do this, it uses "checkpoint" proteins on immune cells, which act like switches that need to be turned on (or off) to start an immune response. Cancer cells sometimes use these checkpoints to keep the immune system from attacking them. But drugs that target these checkpoints hold a lot of promise as cancer treatments.
Drugs called checkpoint inhibitors can be used for people whose pancreatic cancer cells have tested positive for specific gene changes, such as a high level of microsatellite instability (MSI-H), or changes in one of the mismatch repair (MMR) genes. Changes in MSI or in MMR genes (or both) are often seen in people with Lynch syndrome.
The drugs are used for people whose cancer starts growing again after chemotherapy. They might also be used to treat people whose cancer can't be removed with surgery, has come back (recurred) after treatment, or has spread to other parts of the body (metastasized).
PD-1 inhibitor
Pembrolizumab (Keytruda) is a drug that targets PD-1, a checkpoint protein on immune system cells called T cells, that normally helps keep these cells from attacking normal cells in the body. By blocking PD-1, this drug boosts the immune response against pancreatic cancer cells and can often shrink tumors. This drug is given as an intravenous (IV) infusion.
Our experts providing pancreatic cancer treatment in Bangalore using the latest in evidence-based and minimally invasive surgical techniques.
Our Doctors
Dr. Dinesh M G
Specialty: Surgical Oncologist & Laparoscopic Oncosurgeon
Dr. Dinesh M G, is an efficient surgeon specialized in oncology committed to the care and improvement of quality of life of cancer patients. His exceptional surgical skills, teamwork and knowledge are laudable. He is skilled in performing various minimal access oncologic surgeries and has mastered complex open surgeries in the field of oncology.
Completing MBBS from KIMS, Bangalore followed by MS - General Surgery from JJM Medical College, Davangere and M. Ch - Surgical Oncology from Kidwai Memorial Institute of Oncology, he has a Fellowship in Minimal Access Oncology from Basavatarakam Indo American Cancer Institute.

