What is cervical cancer?
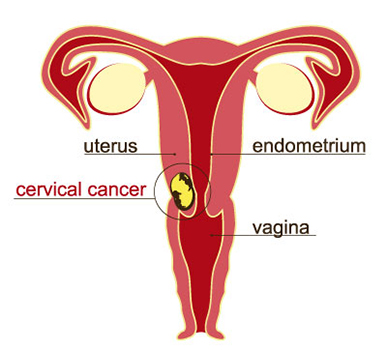
Cervical cancer is a type of cancer that develops in the cells of the cervix, i.e., the lower part of the uterus that connects to the vagina. Cancer starts when cells in the body begin to grow out of control. The cervix is made of two parts and is covered with two different types of cells. The place where these two cell types meet in the cervix is called the transformation zone. Most cervical cancers begin in the cells in the transformation zone.
CAN-C: One of the best cancer centres (in Bangalore) for cervical cancer.
Here, you will find information about signs and symptoms, causes and risk factors, types, diagnosis, staging and prevention about cervical cancer.
Cervical cancer does not usually cause symptoms until it is in the advanced stages. In the early stages of cervical cancer, a person may experience no symptoms at all. The most common symptoms are:
Abnormal vaginal bleeding after intercourse, bleeding after menopause or bleeding and spotting between periods, bleeding after a pelvic exam, or having menstrual periods that are longer or heavier than usual, or also bleeding after douching
Discharge that is unusual from the vagina in amount, colour, consistency, or smell, also watery, bloody, vaginal discharge with strong odour that may contain some blood and may be heavy
Pelvic pain or pain and discomfort during intercourse
Urinating more frequently
Painful urination
Pelvic pain not related to your menstrual cycle
Signs and symptoms seen with more advanced disease can include:
Swelling of the legs
Problems urinating or having a bowel movement
Blood in the urine
We are one of the Bangalore's leading cancer treatment centre for people with cervical cancer.
A risk factor is anything that increases your chance of getting a disease such as cancer. Several risk factors can increase your chance of developing cervical cancer. Women without any of these risk factors rarely develop cervical cancer. There are a few risk factors which probably can be changed and a few which cannot be changed.
Risk factors of cervical cancer are:
Human papillomavirus (HPV) infection: Infection by the human papillomavirus (HPV) is the most important risk factor for cervical cancer. Certain types of HPV may cause warts on or around the female genital organs and in the anal area.
Sexual history: Several factors related to your sexual history can increase the risk of cervical cancer. The risk is most likely affected by increasing the chances of exposure to HPV.
Smoking: Women who smoke are about twice as likely as non-smokers to get cervical cancer. It is believed that some substances damage the DNA of cervix cells and may contribute to the development of cervical cancer. Smoking also makes the immune system less effective in fighting HPV infections.
Having a weakened immune system: Human immunodeficiency virus (HIV), the virus that causes AIDS, weakens the immune system and puts people at higher risk for HPV infections. The immune system is important in destroying cancer cells and slowing their growth and spread. In women with HIV, a cervical pre-cancer might develop into an invasive cancer faster than it normally would. Another group of women at risk for cervical cancer are those taking drugs to suppress their immune response, such as those being treated for an autoimmune disease or those who have had an organ transplant.
Chlamydia infection: Chlamydia is a relatively common kind of bacteria that can infect the reproductive system. It is spread by sexual contact. Chlamydia infection can cause pelvic inflammation, leading to infertility.
Long-term use of oral contraceptives (birth control pills): Taking oral contraceptives (OCs) for a long time increases the risk of cancer of the cervix. The risk of cervical cancer goes up the longer a woman takes OCs, but the risk goes back down again after the OCs are stopped, and returns to normal many years after stopping.
Having multiple full-term pregnancies: Women who have had 3 or more full-term pregnancies have an increased risk of developing cervical cancer. It is thought this is probably due to the increased exposure to HPV infection with sexual activity.
Young age at first full-term pregnancy: Women who were younger than 20 years when they had their first full-term pregnancy are more likely to get cervical cancer later in life than women who waited to get pregnant until they were 25 years or older.
A diet low in fruits and vegetables: Women whose diets do not include enough fruits and vegetables may be at increased risk for cervical cancer.
The main types of cervical cancer are:
Squamous cell carcinoma: This type of cervical cancer begins in the thin, flat cells (squamous cells) lining the outer part of the cervix, which projects into the vagina. Most cervical cancers are squamous cell carcinomas. These cancers develop from cells in the exocervix. Squamous cell carcinomas most often begin in the transformation zone.
Adenocarcinoma: This type of cervical cancer begins in the column-shaped glandular cells that line the cervical canal. Most of the other cervical cancers are adenocarcinomas. Adenocarcinomas are cancers that develop from glandular cells. Cervical adenocarcinoma develops from the mucus-producing gland cells of the endocervix.
Adenosquamous carcinomas or mixed carcinomas: Less commonly, cervical cancers have features of both squamous cell carcinomas and adenocarcinomas.
Small cell cancer: Small cell cancer of the cervix is a very rare type of cervical cancer. Small cell cancers tend to grow quickly and are treated in a different way to the more common types of cervical cancer.
Other types of cancer also can develop in the cervix. These other types, such as melanoma, sarcoma, and lymphoma, occur more commonly in other parts of the body.
Screening tests can help detect cervical cancer and precancerous cells that may one day develop into cervical cancer.
Screening tests include:
Pap test: A Pap test can detect abnormal cells in the cervix, including cancer cells and cells that show changes that increase the risk of cervical cancer.
HPV DNA test: The HPV DNA test involves testing cells collected from the cervix for infection with any of the types of HPV that are most likely to lead to cervical cancer.
Colposcopy: Colposcopy can also be used to help guide a biopsy of the cervix. A special instrument called a colposcope is used. The colposcope magnifies the cells of the cervix and vagina, similar to a microscope.
Blood tests:
a. Biopsy: Several types of biopsies can be used to diagnose cervical pre-cancers and cancers. Colposcopic biopsy, Cone biopsy are used
X-ray: An x-ray is a way to create a picture of the structures inside of the body using a small amount of radiation.
Computed tomography (CT or CAT) scan: A CT scan takes pictures of the inside of the body using x-rays taken from different angles. A CT scan can be used to measure the tumor's size.
Magnetic resonance imaging (MRI): An MRI uses magnetic fields, not x-rays, to produce detailed images of the body. MRI can be used to measure the tumor's size.
Positron emission tomography (PET) or PET-CT scan: A PET scan is usually combined with a CT scan (see above), called a PET-CT scan. A PET scan is a way to create pictures of organs and tissues inside the body.
Staging is a measurement of how far the cancer has spread. This is called staging. After all the tests have been completed and the results are known, it should be possible to tell what stage the cancer is. The higher the stage, the further the cancer has spread. Working out the stage of a cancer is important, as it helps a person decide the most effective type of treatment.
Cervical cancer is staged using the TNM system:
T (tumor): This describes the size of the original tumor.
N (node): This indicates whether the cancer is present in the lymph nodes.
M (metastasis): This refers to whether cancer has spread to other parts of the body.
CAN-C: Most up-to-date centre for cervical cancer treatment in Bangalore.
Some of the ways to reduce your risk of cervical cancer:
Receiving a vaccination to prevent HPV infection: It may reduce your risk of cervical cancer and other HPV-related cancers.
Have routine Pap tests: Pap tests can detect precancerous conditions of the cervix, so they can be monitored or treated in order to prevent cervical cancer.
Practice safe sex: Practising safe sex such as using a condom every time and limiting the number of sexual partners.
Do not smoke: Not smoking is another important way to reduce the risk of cervical pre-cancer and cancer.
"CAN-C: Specialized centre for cervical cancer treatment in Bangalore."
Make An Appointment Today
How Cervical Cancer is treated?
If you've been diagnosed with cervical cancer, it is necessary to know about treatment options. The treatment of cervical cancer depends on several factors, including the type and stage of cancer, possible side effects, and the woman's preferences and overall health. Surgery, radiation, chemotherapy, targeted therapy, immunotherapy or a combination of the these may be used.
Many women with cervical cancer will have some type of surgery. Surgery can be used to: help diagnose cervical cancer, help determine how far the cancer has spread, help treat the cancer (especially for early-stage cancers).
Surgery for cervical pre-cancers:
Two types of procedures can be used to treat pre-cancers of the cervix:
a. Ablation destroys cervical tissue with cold temperatures or with a laser rather than removing it.
b. Excisional surgery (conization) cuts out and removes the pre-cancer.
1. Cryosurgery: Cryosurgery is a type of ablation where a very cold metal probe is placed directly on the cervix. This kills the abnormal cells by freezing them. It is used to treat cervical intraepithelial neoplasia.
2. Laser ablation: It directs a focused laser beam through the vagina to vaporize abnormal cells. It is also used to treat cervical intraepithelial neoplasia.
3. Conization: Another way to treat cervical intraepithelial neoplasia is with excisional surgery called conization. It is used as a treatment since it can sometimes completely remove pre-cancers and some very early cancers.
Surgery for invasive cervical cancer:
Procedures to treat invasive cervical cancer are:
a. Hysterectomy (simple or radical)
b. Trachelectomy
1. Simple hysterectomy: A simple hysterectomy removes the uterus (both the body of the uterus and the cervix) but not the structures next to the uterus. It is used to treat certain types of severe CIN or certain types of very early cervical cancer. There are different ways to do a hysterectomy: Abdominal hysterectomy, Vaginal hysterectomy, Laparoscopic hysterectomy, Robotic-assisted surgery.
2. Radical hysterectomy: For this operation, the surgeon removes the uterus along with the tissues next to the uterus, the cervix, and the upper part of the vagina next to the cervix. More tissue is removed in a radical hysterectomy than in a simple one. Some lymph nodes will also be removed and checked for cancer at this time.
3. Trachelectomy: A radical trachelectomy, allows women to be treated without losing their ability to have children. The operation is done either through the vagina or the abdomen, and is sometimes done using laparoscopy.
4. Pelvic exenteration: This operation is done for very specific cases of recurrent cervical cancer. In this surgery, all of the same organs and tissues are removed as in a radical hysterectomy with pelvic lymph node dissection. In addition, the bladder, vagina, rectum, and part of the colon is also removed, depending on where the cancer has spread.
Surgery to remove nearby lymph nodes:
1. Para-aortic lymph node sampling: Usually during surgery for a radical hysterectomy, the lymph nodes next to the aorta (the large artery in the abdomen) are removed. This is called para-aortic lymph node sampling.
2. Pelvic lymph node dissection: Cancer that starts in the cervix can spread to lymph nodes (pea-sized collections of immune system cells) in the pelvis. To check for lymph node spread, the surgeon might remove some of these lymph nodes. This procedure is known as a pelvic lymph node dissection or lymph node sampling. It is done at the same time as a hysterectomy or trachelectomy.
3. Sentinel lymph node mapping and biopsy: Sentinel lymph node mapping and biopsy is a procedure in which the surgeon finds and removes only the lymph node(s) where the cancer would likely spread first.
Radiation therapy uses high energy x-rays to kill cancer cells. Depending on the stage of the cervical cancer, radiation therapy may be used:
1. As a part of the main treatment: For some stages of cervical cancer, the preferred treatment is radiation alone or surgery followed by radiation. For other stages, radiation and chemo given together (called concurrent chemoradiation) is the preferred treatment as the chemo helps the radiation work better.
2. To treat cervical cancer that has spread or that has come back after treatment: Radiation therapy may be used to treat cervical cancers that have spread to other organs and tissues.
The types of radiation therapy most often used to treat cervical cancer are:
1. External beam radiation, (EBRT): It aims x-rays at the cancer from a machine outside the body. Treatment is much like getting a regular x-ray, but the radiation dose is stronger. When EBRT is used as the main treatment for cervical cancer, it is usually combined with chemotherapy (called concurrent chemoradiation).
2. Brachytherapy: It is also known as internal radiation therapy, puts a source of radiation in or near the cancer. This type of radiation only travels a short distance. The type of brachytherapy used most often to treat cervical cancer is known as intracavitary brachytherapy. The radiation source is placed in a device in the vagina (and sometimes in the cervix). Brachytherapy is mainly used in addition to EBRT as a part of the main treatment for cervical cancer. Rarely, it might be used alone in very specific cases of early-stage cervical cancers. There are two types of brachytherapy: Low-dose rate (LDR) brachytherapy and High-dose rate (HDR) brachytherapy.
We are the leading expert centre for cervical cancer treatment in Bangalore.
Chemotherapy (chemo) uses anti-cancer drugs that are injected into a vein or given by mouth. These drugs enter the bloodstream and can reach almost all areas of the body, making this treatment useful for killing cancer cells in most parts of the body.
As part of the main treatment for cervical cancer:
For some stages of cervical cancer, the preferred treatment is radiation and chemo given together (called concurrent chemoradiation). The chemo helps the radiation work better. Options for concurrent chemoradiation include:
1. Cisplatin given weekly during radiation. This drug is given into a vein (IV). (If cisplatin is not a good option, carboplatin may be used instead.)
2. Cisplatin plus 5-fluorouracil (5-FU) given every 3 weeks during radiation.
The chemo drugs most often used to treat cervical cancer that has come back or spread to other areas include: Cisplatin, Carboplatin, Paclitaxel (Taxol), Topotecan. Combinations of these drugs are often used.
The targeted drugs work differently from standard chemotherapy (chemo) drugs.
Drugs that target blood vessel formation:
1. Vascular endothelial growth factor (VEGF) is a protein that helps tumors form new blood vessels (a process known as angiogenesis) to get nutrients they need to grow. Some targeted drugs called angiogenesis inhibitors stop VEGF from working and block this new blood vessel growth.
2. Bevacizumab (Avastin®) is an angiogenesis inhibitor that can be used to treat advanced cervical cancer. It is a monoclonal antibody (a man-made version of a specific immune system protein) that targets VEGF.
This drug is often used with chemo for a time. Then, if the cancer responds, the chemo may be stopped and the bevacizumab given by itself until the cancer starts growing again.
CAN-C: Your complete cancer treatment centre (in Bangalore) for cervical cancer.
Immunotherapy is the use of medicines to stimulate a person's own immune system to recognize and destroy cancer cells more effectively. Immunotherapy can be used to treat cervical cancer that has spread or come back (recurred).
1. Immune checkpoint inhibitors: An important part of the immune system is its ability to keep itself from attacking the body's normal cells. To do this, it uses "checkpoints" - molecules on immune cells that need to be turned on (or off) to start an immune response. Cancer cells sometimes use these checkpoints to avoid being attacked by the immune system. Newer drugs that target these checkpoints are being used as cancer treatments.
Pembrolizumab (Keytruda) targets PD-1, a protein on immune system cells called T cells that normally helps keep these cells from attacking other cells in the body. By blocking PD-1, these drugs boost the immune response against cancer cells. This can shrink some tumors or slow their growth.
Pembrolizumab can be used for certain types of cervical cancer that start growing again after chemotherapy or that has spread. This immunotherapy drug is given as an intravenous (IV) infusion.
We at CAN-C are the right centre for cervical cancer treatment in Bangalore.
Our Doctors
Dr. Dinesh M G
Specialty: Surgical Oncologist & Laparoscopic Oncosurgeon
Dr. Dinesh M G, is an efficient surgeon specialized in oncology committed to the care and improvement of quality of life of cancer patients. His exceptional surgical skills, teamwork and knowledge are laudable. He is skilled in performing various minimal access oncologic surgeries and has mastered complex open surgeries in the field of oncology.
Completing MBBS from KIMS, Bangalore followed by MS - General Surgery from JJM Medical College, Davangere and M. Ch - Surgical Oncology from Kidwai Memorial Institute of Oncology, he has a Fellowship in Minimal Access Oncology from Basavatarakam Indo American Cancer Institute.

